This is part two of our series focusing on ideas and suggestions for adapting family traditions and caring for yourself, when a loved one has dementia.
By: Lauren Flake
I remember the last time I was able to bring my mother, who had early onset Alzheimer’s disease, to my house on Christmas Eve. It was only a couple of months after my family moved her into the secure wing of a nursing home.
She did well that day because it was a small, calm gathering of only our immediate family—my dad, my brother, my husband, and me. She still basically knew who we all were and could toilet herself with little assistance. After that, however, incorporating my mom into our holiday celebrations became more difficult.
Based on my family’s experience, here are my best tips to get through the holidays with your loved one who has Alzheimer’s or a related dementia:
1. Lower your expectations.
Simplify your celebrations as much as possible in this busy season. Limit chaos for yourself as the care partner and for your loved one with dementia by choosing only a few essential holiday traditions. Let go of extra “should”s and endless to-dos. It’s okay to decline party invitations, to not send out cards, or to not put lights on your house.
2. Bring the holiday festivities to your loved one.
People with dementia almost always function better when they’re in their normal surroundings, like their memory care facility or their home. If you can, bring the party to them. Wherever you choose to celebrate with your loved one, be sure that it is well lit and uncluttered.
3. Talk to children about the disease ahead of time.
Kids, like adults, tend to fear what they don’t understand. Discuss beforehand the behaviors they may see from a relative with dementia. A great resource to prepare children for being around loved ones with Alzheimer’s disease at holiday gatherings is Maria Shriver’s picture book, What’s Happening to Grandpa?.
4. Schedule self-care breaks for yourself.
Be sure to set aside time for yourself in this festive season. Find a respite program for your loved one if you are their primary care partner. Exercise. Get a massage or a pedicure. Talk to a counselor. Go see a funny movie. Go for a walk. Read a novel. Laugh with your best friend.
5. Choose gifts based on the five senses.
The best gifts for people with dementia are often the simplest ones. Keep their five senses in mind when shopping for presents. A few ideas include headphones and an MP3 player loaded with favorite music from their teenage years, hand lotion in a familiar scent like vanilla, poster prints of childhood photos, or a fuzzy blanket.
Getting through the holidays with a loved one with Alzheimer’s or dementia is about being present in each moment, making connections with your loved one, and finding rest for both of you in the chaos of the season.
Lauren Flake is a wife, mom to two girls, watercolor artist, seventh generation Texan, and early onset Alzheimer’s daughter. She is the author and co-illustrator of two award-winning children’s books for grieving preschoolers, Where Did My Sweet Grandma Go? and Where Did My Sweet Grandpa Go?, and the editor of Love of Dixie magazine. She loves green tea, dark chocolate, and collecting all things turquoise. You can find her at LaurenFlake.com.



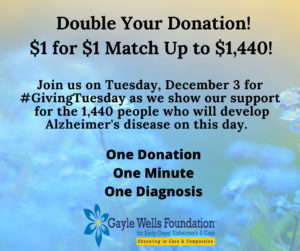 One person…every minute…1,440 people. This is the number of people that will develop Alzheimer’s disease today. This doesn’t take into consideration the numbers of people that will develop other types of dementia today (i.e. Lewy Body, frontotemporal dementia, vascular dementia, and others).
One person…every minute…1,440 people. This is the number of people that will develop Alzheimer’s disease today. This doesn’t take into consideration the numbers of people that will develop other types of dementia today (i.e. Lewy Body, frontotemporal dementia, vascular dementia, and others).