Recent Articles
Holidays & Dementia: Ideas & Suggestions for the Holiday Season – Part Two
This is part two of our series focusing on ideas and suggestions for adapting family traditions and caring for yourself, when a loved one has dementia.
By: Lauren Flake
I remember the last time I was able to bring my mother, who had early onset Alzheimer’s disease, to my house on Christmas Eve. It was only a couple of months after my family moved her into the secure wing of a nursing home.
She did well that day because it was a small, calm gathering of only our immediate family—my dad, my brother, my husband, and me. She still basically knew who we all were and could toilet herself with little assistance. After that, however, incorporating my mom into our holiday celebrations became more difficult.
Based on my family’s experience, here are my best tips to get through the holidays with your loved one who has Alzheimer’s or a related dementia:
1. Lower your expectations.
Simplify your celebrations as much as possible in this busy season. Limit chaos for yourself as the care partner and for your loved one with dementia by choosing only a few essential holiday traditions. Let go of extra “should”s and endless to-dos. It’s okay to decline party invitations, to not send out cards, or to not put lights on your house.
2. Bring the holiday festivities to your loved one.
People with dementia almost always function better when they’re in their normal surroundings, like their memory care facility or their home. If you can, bring the party to them. Wherever you choose to celebrate with your loved one, be sure that it is well lit and uncluttered.
3. Talk to children about the disease ahead of time.
Kids, like adults, tend to fear what they don’t understand. Discuss beforehand the behaviors they may see from a relative with dementia. A great resource to prepare children for being around loved ones with Alzheimer’s disease at holiday gatherings is Maria Shriver’s picture book, What’s Happening to Grandpa?.
4. Schedule self-care breaks for yourself.
Be sure to set aside time for yourself in this festive season. Find a respite program for your loved one if you are their primary care partner. Exercise. Get a massage or a pedicure. Talk to a counselor. Go see a funny movie. Go for a walk. Read a novel. Laugh with your best friend.
5. Choose gifts based on the five senses.
The best gifts for people with dementia are often the simplest ones. Keep their five senses in mind when shopping for presents. A few ideas include headphones and an MP3 player loaded with favorite music from their teenage years, hand lotion in a familiar scent like vanilla, poster prints of childhood photos, or a fuzzy blanket.
Getting through the holidays with a loved one with Alzheimer’s or dementia is about being present in each moment, making connections with your loved one, and finding rest for both of you in the chaos of the season.
Lauren Flake is a wife, mom to two girls, watercolor artist, seventh generation Texan, and early onset Alzheimer’s daughter. She is the author and co-illustrator of two award-winning children’s books for grieving preschoolers, Where Did My Sweet Grandma Go? and Where Did My Sweet Grandpa Go?, and the editor of Love of Dixie magazine. She loves green tea, dark chocolate, and collecting all things turquoise. You can find her at LaurenFlake.com.
Holidays & Dementia: Ideas and Suggestions for the Holiday Season – Part One
This is part one of a two-part series focusing on ideas and suggestions for adapting family traditions and caring for yourself, when a loved one has dementia.
By: Todd Wagoner, MSW, LCSW
While the holiday season is a time for celebration and joy, many care partners supporting loved ones with dementia may feel added stress to maintain traditions while also providing care. To help, The Gayle Wells Foundation for Early Onset Alzheimer’s & Care offers the following strategies to help support care partners this holiday season.
Give yourself permission to under-commit. Under normal, non-care partner circumstances, it’s easy to overcommit during the holiday season, but the pressure is even greater for care partners. Psychologist and author, Dr. Barry Jacbos, PsyD, writes, “Caregivers notoriously overcommit themselves and then feel trapped by promises they’ve made that slowly break them.”1
As a care partner, talking to family members can help set realistic expectations about holiday celebrations, enable discussion for ways to shift responsibilities to continue traditions, or brainstorm ways to make their celebrations more manageable for the care partner and person with dementia.
Here are a few suggestions for the care partner and family members when having a family discussion:
- Reflect and prepare: Make a list of key talking points before the discussion so both the care partner and family have outlined their thoughts and goals before the meeting. Writing this information out helps organize one’s thoughts, clarify any potential misconceptions, and help to create an agenda for the discussion.
- Approach with love and concern: Make sure your mind and expectations are in the right place to set the tone for the discussion. Author and speaker, Amy Goyer, notes in her book Juggling Life, Work, and Caregiving, to caution families not to approach a group discussion with a “negative and confrontational attitude.” This allows the family to approach the discussion with a common goal of focusing on the needs of the care recipient and care partner.
- Listen and validate: Listen to what others have to say with an open mind, and reflect or repeat their own thoughts and ideas to show you’re hearing them. Family members (particularly care partners) might feel scared, angry, confused, or hopeless, so it’s important to remain compassionate and supportive.
- Include key people in the conversation: Goyer also suggests when having a family meeting to make sure key family members are in the conversation. Some families may benefit in having a third party such as a family physician or care manager to help mediate or guide the conversation, if this is helpful.
Embrace the new normal. While traditions are an important aspect of the holidays, making sure everyone can enjoy and participate in the celebration should take priority. Large gatherings can be noisy and chaotic, which can increase irritability and agitation in a person with dementia and cause stress for the care partner.
Remaining mindful of the care recipient’s energy level and interactions while maintaining their daily routine as much as possible helps to create an enjoyable atmosphere for all. Having a more intimate gathering at the care recipient’s home for a shorter period of time allows the person with dementia to participate in a way that’s comfortable for them.
Don’t feel pressured by the past. As a care partner, it’s important not to compare past holiday memories to what is possible presently. Geropsychologist Dr. Natali Edmonds, PsyD, explains that care partners create added stress for themselves when they compare how “things used to be to how things are now.” Instead, think about ways to build on those past traditions in a way that’s manageable.
This can include:
- Singing holiday songs familiar to the person with dementia
- Watching a favorite holiday movie together
- Baking cookies or wrapping gifts
- Create a photo album of past holidays and sharing memories
This not only helps the person with dementia participate in a way that’s comfortable for them, but it also helps create new and lasting positive memories for everyone in the process.
Taking the time to have these conversations and allowing the care partner the space to be “present in the moment” lets everyone find holiday joy while making new traditions together.
1 Jacbos, Barry. The Emotional Survival Guide for Caregivers: Looking After Yourself and Your Family While Helping an Aging Parent
Todd Wagoner is a Master’s level clinical social worker with over 25 years of health care experience in hospital discharge planning and, most recently, serving as geriatric social worker for the Touchpoint Healthy Aging Transition Services, a geriatric specialty clinic through the Community Health Network in Noblesville, Indiana.
1,440 People Will Develop Alzheimer’s Disease Today
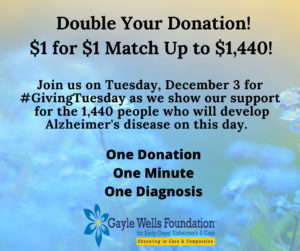 One person…every minute…1,440 people. This is the number of people that will develop Alzheimer’s disease today. This doesn’t take into consideration the numbers of people that will develop other types of dementia today (i.e. Lewy Body, frontotemporal dementia, vascular dementia, and others).
One person…every minute…1,440 people. This is the number of people that will develop Alzheimer’s disease today. This doesn’t take into consideration the numbers of people that will develop other types of dementia today (i.e. Lewy Body, frontotemporal dementia, vascular dementia, and others).
This disease is personal to me as I know it is to many of you reading this post. On this #GivingTuesday, the Gayle Wells Foundation for Early Onset Alzheimer’s & Care would like to raise $1,440 to honor those whose lives will be forever changed on this day. Due to the generosity of an anonymous donor, gifts will be matched $1 for $1 up to $1,440. A gift of $5 doubles to $10!
Please consider supporting our efforts as we provide one-on-one support, care, and education to individuals, their families, and their communities at no cost. Click here to access our #GivingTuesday fundraising page. #forgetmenotgwf #earlyonsetAlz
Thank you,
Laura Sutherland
Founder & Executive Director
The Power of Communication in Early Onset Alzheimer’s Disease
Written by: Melinda Mattson
Memory Care Advocate & Board Member, Gayle Wells Foundation for Early Onset Alzheimer’s & Care
Meaningful communication is at the heart of every trusted relationship, which is what makes the loss of conversation through early onset Alzheimer’s disease especially painful. But with a bit of knowledge and creativity, we can still have meaningful connection with our loved ones.
The first step is to understand the process of the disease’s impact on communication. While every individual’s experience with early onset Alzheimer’s disease is different, it is common for those affected to forget important events, call things by the wrong name, or forget words. With this in mind, we need to be prepared to find a new approach to interaction.
We also need to consider the context of the conversation. Face to face is ideal since the phone can present another level of confusion for the individual with early onset Alzheimer’s disease. Video chats are one alternative for those who wish to connect from afar.
Ultimately, respect needs to remain at the heart of each of our interactions. Seeking first to understand before trying to be understood will be our golden rule as we approach conversation. While we may not always understand what our loved ones are trying to communicate, we can sympathize with the challenge they face in struggling to be understood.
Our job is not to make them understand. We may not be able to do this nor is it our charge. Our role is to lean in, listen, and offer our reassuring presence. Even if what they are saying isn’t aligned with facts or reality, their feelings and experience are real to them and worthy of dignity.
Refrain from arguing or correcting. Pointing out mistakes to an individual with early onset Alzheimer’s disease often erodes trust and increases frustration and embarrassment for them.
The litmus test in correcting an individual with early onset Alzheimer’s disease is to ask if their line of thinking will harm them or others. If not, let it go and meet them where they are.
The key to connecting with individuals with early onset Alzheimer’s disease is to remember they are still with us. Because we no longer talk in the ways we used to, it’s easy to assume they aren’t available. But indeed, they are, we’ll just need to be a bit more creative to reach them.
Just as you would approach anyone who experienced trauma with gentleness and respect, so we should with those experiencing forms of dementia. Losing any portion of mental function is frightening and traumatic for anyone. Our approach must be filled with the utmost care and tenderness.
Consider these suggestions as you engage in conversation:
- Introduce yourself as you enter the room. Call the individual by name and make eye contact.
- Speak directly to them and not to a caregiver about them in their presence.
- If possible, carry on a one-on-one conversation without the distraction of other conversations, radio, or TV.
- Speak in a dignified tone, not in baby talk.
- Gently hold their hand or touch their arm as you speak.
- When asking questions, limit the answer choices instead of asking open ended questions. For example, ask “Would you like a water to drink?” Rather than, “What would you like to drink?”
- Give simple one-step instructions. Gesture or point to objects for reference. Use pictures to help them reminisce.
- Be exceedingly patient and positive with mistakes. Instead of correcting, use positive language such as “Let’s try it this way.”
- Pay attention to non-verbal cues. Is your loved one excited or upset? Even if you’re unsure of the words they are saying, sympathize with the emotions they’re displaying.
- Reassure, reassure, reassure. Praise their efforts without condescension and patiently wait for them to find their words.
- Do not say “I told you this already,” or “Don’t you remember?”
- If they’re unable to find the words, offer suggestions. “Are you trying to tell me you want your sweater?” If you’re still not understanding their request, ask if they’d like to write a note or point to what they want.
- If they speak of non-sensical things or incorrectly recall dates or events, resist the urge to correct them.
- If they are enjoying a conversation about a made-up event or person, join them. While it may feel uncomfortable at first, allowing them the pleasure of conversation is the point.
- If conversation isn’t working on a given day, offer your quiet presence as a gift to them. Try again another day.
- If your loved one is non-verbal, remember your presence and company communicates care and love. Gentle physical touch and meaningful eye contact often speak more than words.
We appreciate the immense sadness and grief associated with failed attempts to communicate with your loved ones. We are committed to providing the best resources to you to help you meet these challenges and connect with your beloved.
Let us hear from you if you have found methods to reach your loved one. We are better together.
Sources:
Mayo Clinic: Tips for Better Communication
Aspired Living: Overcoming Communication Barriers
What is Early Onset Alzheimer’s Disease
Written by: Laura Sutherland & Sara Wuillermin
What Is Early Onset Alzheimer’s Disease?
Early onset Alzheimer’s disease is a form of dementia that affects people in their 30s through early 60s. While most individuals with Alzheimer’s disease are diagnosed with late onset Alzheimer’s (65 years of age and older) the number of cases of early onset Alzheimer’s disease is increasing. It is estimated by some researchers that at least 10% of Alzheimer’s cases are early onset, which equates to approximately 500,000 individuals.
What Are the Symptoms of Early Onset Alzheimer’s Disease?
Alzheimer’s disease impacts the brain in many ways beyond forgetfulness and the inability to recognize people. Some of the first indicators of early onset Alzheimer’s disease can be a progression of changes that may include:
- Emotional Responses: Increased anger or irritation, emotional outbursts, sadness, tearfulness
- Social Behavior: Withdrawing from friends, family, activities; increased dependence on others
- Financial decision-making: Difficulties managing money, paying bills, writing checks, using credit cards
- Transportation/Navigational Abilities: Getting lost; issues with driving or public transportation; wandering
- Job and Home Responsibilities: Difficulties with job performance; inability to complete tasks such as feeding pets, cooking, household chores
- Personal Care: Struggling to maintain personal hygiene and dressing; changes in eating habits
- Memory: Forgetfulness, repeating questions, misplacing objects, missing appointments
- Communication: Difficulty finding appropriate words, inability to follow conversation, losing train of thought
What to Do If I Think Someone I Love, or Myself, Might Have Early Onset Alzheimer’s?
If you, or a loved one, are consistently experiencing any of the above symptoms, schedule a comprehensive medical evaluation with your primary care physician and possibly a neurologist or other specialist.
In preparing for your appointment, make sure to:
- Review Preparing for the Doctor’s Appointment
- Complete the Checklist of Common Symptoms/Changes of Early Onset Alzheimer’s Disease
- Complete the Personal Medication Record
- Complete the Health History Record
Please take your time and be thorough and honest about all symptoms, medications, and health history. Accurate recording of symptoms/changes will help you or your loved one’s medical and care teams determine the best possible treatment, programs, and services to meet the needs throughout the course of the disease.
How Do You Diagnose Early Onset Alzheimer’s?
Obtaining a diagnosis of early onset Alzheimer’s disease can be difficult. Due to a person’s young age and healthy appearance, physicians will often first explore other potential causes for the described symptoms. Early stage evaluations might point to stress, depression, menopause, B-12 deficiency, or other illnesses. It is not uncommon for someone to see 2 to 3 doctors before receiving an accurate diagnosis. Due to these difficulties, individuals with early onset Alzheimer’s may not necessarily be in the early stages of the disease when they receive the diagnosis.
We understand the anxiety, fear, and stress associated with going to the doctor and wondering what they will diagnose. To help alleviate some of the unknown, we have provided a list of common Diagnostic Tests for Early Onset Alzheimer’s that might be used/ordered during your visit. Please note that doctors may not utilize all these tools or may order additional tests that are not listed.
Our Beliefs and Resources for Early Onset Alzheimer’s Disease
The Gayle Wells Foundation for Early Onset Alzheimer’s & Care believes each person with early onset Alzheimer’s disease is a unique individual and should be treated as such. We believe in the importance of understanding a person’s history so that we can provide person-centered care. This is crucial in allowing the person to maintain their identity throughout the disease process. We also understand the sacrifice care partners make when they step into the unknown world of caring for a loved one with early onset Alzheimer’s disease. We believe that all care partners should have access to one-on-one education and training on a continual basis as they navigate the different aspects of this disease.
We provide care consultations, support groups, one-on-one education & training for those with the disease, their care partners, children, family, and friends. Please fill out the Contact Us form with your information and we will respond to you within 24 hours. Our services are at no cost and we will walk this journey with you and provide consistent support and reassurance.
The Gayle Wells Foundation Announces Early Onset Alzheimer’s Awareness Day
The Gayle Wells Foundation for Early Onset Alzheimer’s Disease & Care (GWF) is proud to announce that the first nationwide Early Onset Alzheimer’s Awareness Day will be recognized on September 14.
Early-onset Alzheimer’s disease affects people in their 30s through 60s, and there is no effective treatment or cure. This population is often overlooked because they are considered to be in the minority of those diagnosed with Alzheimer’s disease; however, the number of individuals believed to be living with early onset Alzheimer’s is estimated to be more than 500,000 people in the United States. The challenges they face are numerous, as programs, long-term care facilities, and financial assistance are often structured for individuals older than 65 years of age.
Through the creation of Early Onset Alzheimer’s Awareness Day, we strive to raise awareness for this affected population as we work to increase programs and services specifically geared to those impacted by this disease. We also intend to recognize the unique challenges that individuals and families impacted by early onset Alzheimer’s disease endure.
The date for Early Onset Alzheimer’s Awareness Day, September 14, was chosen in loving memory of Gayle Wells, who died from the disease on this date in 2011. The GWF was created in Gayle’s honor to provide education, training, support, and care to those living with early onset Alzheimer’s disease, their care partners, families, and friends.
The Gayle Wells Foundation for Early Onset Alzheimer’s & Care (GWF) is a 501(c)(3) organization that provides one-on-one support, care planning, education and training for individuals, care partners, children, and the community, at no cost.
If you would like more information about the Gayle Wells Foundation for Early Onset Alzheimer’s & Care, please contact Laura Sutherland, Founder & Executive Director, at 832-470-9526 or laura@gaylewells.org.
End-of-Life Doula Program Being Established
The Gayle Wells Foundation for Early Onset Alzheimer’s & Care (GWF) is establishing an end-of-life doula program that will allow us to provide non-medical care, support, guidance, and comfort to people dying from early onset Alzheimer’s disease, as well as to their families. Sadly, too many people with Alzheimer’s disease die alone and they have not been given the opportunity to express their end of life wishes. Death is viewed as taboo in our society and something no one wants to talk about, yet it is the only thing we all have in common. There is no question that death is frightening, sad, and a very dark and emotional time, but it can also be a time to show love, honor, forgiveness, and support to the dying individual that touched so many lives.
The Gayle Wells Foundation for Early Onset Alzheimer’s & Care (GWF) believes people should be given the opportunity to reflect on their lives and explore the legacy and meaning of their time on this earth. We also believe people have the right to express wishes for their death and be surrounded and supported by their loved ones when that time comes. In addition to guiding our patients and families through their journey with early onset Alzheimer’s disease, we will also be able to continue our guidance and support through end-of-life. We do not take this responsibility lightly and we consider this a tremendous honor. We will begin offering this service in August/September and volunteer trainings will begin in early summer.
If you would like to receive updates on our end-of-life doula program, please sign up for our mailing list by clicking here. We also encourage you to share this information with your friends and communities.
Laura Sutherland
Founder & Executive Director
Historic Breakthrough in the Treatment of Alzheimer’s Disease
Researchers at the West Virginia University’s Rockefeller Neuroscience Institute have successfully performed a phase II trial using focused ultrasound to treat a patient with early onset Alzheimer’s disease. This is exciting news and holds promise for future treatments. The complete article can be accessed by clicking here.
Why are nursing homes drugging dementia patients without their consent?
By Hannah Flamm
August 10, 2018
Now more than ever it is important that we keep watch of our elderly; but also keep watch of those caring for them. It is sad to see homes resorting to these irresponsible action that effect more than just the patient. Hopefully more reports like this will lift the veil and action will be taken accordingly. – GWF
The following is an excerpt from a Washington Post article by Hannah Flamm, with a link to the full article:
It helps control the residents, and institutions are rarely punished.
A year and a half ago in a Texas nursing home, I met an 84-year-old resident with dementia named Felipa Natividad. Her sister, Aurora Suarez, told me that the staff dosed Natividad with Haldol, an antipsychotic drug, to ease the burden of bathing her. “They give my sister medication to sedate her on the days of her shower: Monday, Wednesday, Friday,” Suarez said. “They give her so much she sleeps through the lunch hour and supper.” A review of Natividad’s medical chart confirmed the schedule.
Suarez said she had given her consent to use the drugs because she feared that the staff would not bathe her sister enough if she refused. But when Suarez saw the effect they had, she had second thoughts. She expressed them to the nursing home, but Natividad was taken off the antipsychotics only after she was placed in hospice care. She died a few months after my interview. Her family, seeing her in a reduced state and unable to communicate, wondered whether the drugs had compounded the losses associated with dementia; Suarez thought they… [Continue to full article]
Fall Prevention Tips
Every year, millions of people fall and cause injury to themselves. For the person living with Alzheimer’s disease or other types of dementia, the risk of falling increases as the disease progresses. Depth perception, vision problems, and loss of balance and coordination are contributing factors. A study from the medical journal of Age and Ageing, found that those living with Alzheimer’s are three times more likely to suffer hip fractures from a fall. According to the Centers for Disease Control (CDC), one out of five falls can cause broken bones or a head injury. Head injuries can be extremely serious, especially if the person is taking blood thinners or other medications. Additional medications, such as tranquilizers, sedatives, or antidepressants, as well as some over-the-counter medications can also affect balance and increase the risk of falling.
There are steps you can take create a safe home environment for your loved one. One of the best guides I have come across is the Fall Prevention Guide from Right at Home. This guide outlines risk factors and preventive steps for each room in your home. This guide is applicable for everyone, not just those living with Alzheimer’s. Please click on the guide and feel free to share this information with your family and friends.